Table of Contents
Introduction: IBS Management
Living with Irritable Bowel Syndrome (IBS) can be challenging, with symptoms like bloating, abdominal pain, and unpredictable bowel habits significantly impacting quality of life. If you’re among the millions worldwide struggling with IBS, you’ve likely heard about the low FODMAP diet—an evidence-based approach that has revolutionized IBS management. However, navigating this complex dietary intervention requires understanding, planning, and practical alternatives to maintain both nutritional adequacy and enjoyment in eating.
This comprehensive guide explores everything you need to know about managing IBS through the low FODMAP approach, with special emphasis on practical food alternatives that make the diet sustainable and effective. From understanding the science behind FODMAPs to implementing a personalized plan with delicious alternatives, this resource aims to empower you on your journey toward better digestive health.
Understanding FODMAPs and IBS
What Are FODMAPs?
FODMAP is an acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are specific types of short-chain carbohydrates that share three important characteristics:
- Poor absorption in the small intestine
- High osmotic activity, drawing water into the intestinal lumen
- Rapid fermentation by gut bacteria, producing gas
When these carbohydrates aren’t properly absorbed in the small intestine, they travel to the large intestine where gut bacteria ferment them, producing hydrogen, carbon dioxide, and methane gases. For people with IBS, this process can trigger or worsen symptoms like bloating, abdominal pain, flatulence, and altered bowel habits.
The main categories of FODMAPs include:
- Oligosaccharides: Found in wheat, rye, legumes, and some vegetables (like onions and garlic)
- Disaccharides: Primarily lactose, found in dairy products
- Monosaccharides: Mainly fructose, found in honey, apples, and high fructose corn syrup
- Polyols: Sugar alcohols like sorbitol and mannitol, found in some fruits and vegetables, as well as artificial sweeteners
The Science Behind FODMAPs and IBS
The connection between FODMAPs and IBS symptoms has been extensively researched, particularly by scientists at Monash University in Australia, who pioneered the low FODMAP approach. Studies have consistently shown that FODMAPs can trigger IBS symptoms through several mechanisms:
- Luminal Distension: The osmotic effect of FODMAPs draws water into the intestine, while their fermentation produces gas. Together, these effects stretch the intestinal wall, triggering pain and discomfort in sensitive individuals.
- Visceral Hypersensitivity: People with IBS often have heightened sensitivity to normal digestive processes. Even normal amounts of gas or intestinal stretching can cause significant discomfort.
- Altered Gut Microbiota: FODMAPs influence the composition and function of gut bacteria, which may contribute to IBS symptoms in susceptible individuals.
- Increased Intestinal Permeability: Some research suggests FODMAPs may affect gut barrier function, potentially contributing to IBS symptoms.
- Production of Short-Chain Fatty Acids (SCFAs): While SCFAs are generally beneficial for gut health, their production during FODMAP fermentation may contribute to symptoms in IBS patients.
Research published in 2013 from Monash University demonstrated that up to 86% of IBS patients achieved relief of overall gastrointestinal symptoms through the low FODMAP approach, particularly for bloating, flatulence, abdominal pain, and altered bowel habits.
The Low FODMAP Diet Approach
Three-Phase Process
The low FODMAP diet is not intended as a lifelong restrictive diet but rather as a process to identify and manage trigger foods. It follows a structured three-phase approach:

Phase 1: Low FODMAP (Restriction)
This initial phase involves swapping high FODMAP foods for low FODMAP alternatives for a limited period, typically 2-6 weeks. Monash University emphasizes that this is a substitution rather than elimination phase—the goal is to find alternatives, not simply remove foods from your diet.
During this phase, you’ll:
- Learn to identify high and low FODMAP foods
- Substitute high FODMAP foods with suitable alternatives
- Monitor your symptoms to assess improvement
- Work with a dietitian to ensure nutritional adequacy
Phase 2: Reintroduction
Once symptoms have improved, you’ll systematically reintroduce FODMAP subgroups one at a time to identify your specific triggers. This phase typically lasts 6-8 weeks and should be guided by a registered dietitian.
The reintroduction process helps determine:
- Which FODMAP subgroups trigger your symptoms
- Your personal tolerance thresholds for different FODMAPs
- How quickly symptoms appear after consuming trigger foods
- The cumulative effect of consuming multiple FODMAP-containing foods
Phase 3: Personalization
Also known as the maintenance phase, this involves returning to as normal a diet as possible, limiting only the specific FODMAP foods that trigger your symptoms. The goal is to achieve the least restrictive diet that still manages symptoms effectively.
Eventually, some people may be able to incorporate all or most FODMAPs back into their diet without symptoms, particularly as gut health improves over time.
Importance of Professional Guidance
While the low FODMAP diet has proven effective for many IBS sufferers, it’s complex and potentially restrictive. Working with a registered dietitian who specializes in digestive health is strongly recommended for several reasons:
- nutritional Adequacy: Ensuring you maintain adequate nutrition during the restriction phase
- Proper Implementation: Guidance on correctly following each phase
- Personalized Approach: Tailoring the diet to your specific needs and lifestyle
- Preventing Disordered Eating: Monitoring for unhealthy relationships with food
- Long-term Strategy: Developing sustainable eating patterns beyond the initial phases
As noted in recent research, the low FODMAP diet should not be followed for more than 6 weeks in its restrictive phase due to potential nutritional deficiencies and impacts on the gut microbiome.
Comprehensive FODMAP Food Alternatives
One of the most challenging aspects of following a low FODMAP diet is finding suitable alternatives for favorite foods. The good news is that with some knowledge and creativity, you can still enjoy delicious, varied meals while managing IBS symptoms. Here’s a comprehensive guide to FODMAP alternatives across major food categories:
Fruits
| High FODMAP Fruits (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Apples | Firm (unripe) bananas |
| Pears | Oranges |
| Mangoes | Kiwi |
| Watermelon | Grapes |
| Cherries | Strawberries |
| Nectarines | Blueberries |
| Peaches | Raspberries |
| Plums | Grapefruit |
| Blackberries | Cantaloupe (small amounts) |
| Boysenberries | Lemon/Lime |
| Apricots | Mandarin |
| Nashi pears | Passionfruit |
| Persimmon | Rhubarb |
Tips for Fruit Consumption:
- Portion size matters—even low FODMAP fruits can become high FODMAP in large quantities
- Unripe bananas are low FODMAP, while ripe (yellow with brown spots) bananas are high in FODMAPs
- Frozen berries are a convenient and often more affordable alternative to fresh
- Citrus fruits are generally well-tolerated and make excellent flavor enhancers
Vegetables
| High FODMAP Vegetables (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Onions | Green parts of spring onions/leeks |
| Garlic | Garlic-infused oil |
| Cauliflower | Broccoli (small amounts) |
| Mushrooms | Carrots |
| Artichokes | Spinach |
| Asparagus | Zucchini |
| Sugar snap peas | Bell peppers |
| Beetroot | Cucumber |
| Celery (large amounts) | Eggplant |
| Leek bulb | Lettuce |
| Sweet corn | Tomatoes |
| Potatoes | |
| Green beans |
Tips for Vegetable Preparation:
- Garlic-infused oil is a game-changer for flavoring dishes without the FODMAPs (fructans are water-soluble, not oil-soluble)
- Products like Free FOD garlic and onion replacers can help maintain flavor in dishes
- The green parts of spring onions and leeks are low FODMAP and can provide onion-like flavor
- Herbs and spices are generally low FODMAP and can add significant flavor to compensate for the absence of onion and garlic
Grains and Cereals
| High FODMAP Grains (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Wheat-based bread | Gluten-free bread |
| Regular pasta | Gluten-free pasta |
| Couscous | Rice |
| Barley | Quinoa |
| Rye | Oats |
| High FODMAP cereals | Corn-based products |
| Buckwheat | |
| Millet | |
| Rice cakes | |
| Certified low FODMAP cereals |
Tips for Grain Consumption:
- Oats are naturally low FODMAP and make an excellent breakfast option
- Look for certified low FODMAP products like specific Kellogg’s cereals (Cornflakes, Rice Bubbles)
- Sourdough spelt bread may be tolerated better than regular wheat bread as the fermentation process reduces FODMAP content
- Portion size is important—even low FODMAP grains can cause symptoms in large amounts
Dairy and Alternatives
| High FODMAP Dairy (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Regular milk | Lactose-free milk |
| Regular yogurt | Lactose-free yogurt |
| Soft cheeses | Hard cheeses (cheddar, parmesan) |
| Ice cream | Lactose-free ice cream |
| Custard | Almond milk |
| Rice milk | |
| Coconut milk (small amounts) | |
| Cottage cheese (small amounts) |
Tips for Dairy Consumption:
- Lactose is the FODMAP in dairy, but many dairy products naturally contain little lactose
- Hard, aged cheeses like cheddar and parmesan are naturally low in lactose
- Plant-based milk alternatives vary in FODMAP content—almond and rice milk are generally safe options
- Be cautious with oat milk, as some brands may contain high FODMAP ingredients
Protein Sources
| High FODMAP Proteins (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Legumes (beans, lentils, chickpeas) | Canned lentils (rinsed well) |
| Processed meats with garlic/onion | Firm tofu |
| Some marinated meats | Plain meat (beef, chicken, pork) |
| Fish and seafood | |
| Eggs | |
| Tempeh | |
| Plain, unmarinated meats |
Tips for Protein Consumption:
- Plain meats without marinades are generally safe
- Read labels carefully on processed meats, which often contain garlic and onion
- Canned lentils are lower in FODMAPs than dried lentils because some FODMAPs leach into the canning water (rinse well before using)
- Firm tofu is low FODMAP, while silken tofu is high FODMAP
Nuts and Seeds
| High FODMAP Nuts (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Cashews | Peanuts |
| Pistachios | Macadamias |
| Walnuts | |
| Pecans | |
| Pine nuts | |
| Almonds (10 or fewer) | |
| Pumpkin seeds | |
| Sunflower seeds | |
| Chia seeds | |
| Flaxseeds |
Tips for Nuts and Seeds Consumption:
- Portion size is crucial—even low FODMAP nuts can become high FODMAP in large quantities
- Almonds are low FODMAP in small portions (10 or fewer)
- Nut butters made from low FODMAP nuts are generally safe in appropriate portions
- Seeds are excellent sources of nutrients and are generally well-tolerated in moderate amounts
Sweeteners and Condiments
| High FODMAP Sweeteners/Condiments (To Avoid) | Low FODMAP Alternatives |
|---|---|
| High fructose corn syrup | Maple syrup (in moderation) |
| Honey | Stevia |
| Agave nectar | Sucrose (table sugar) |
| Sorbitol, mannitol, xylitol | Brown sugar |
| Garlic and onion-based condiments | Glucose |
| Aspartame | |
| Mustard | |
| Fish sauce | |
| Soy sauce (check ingredients) | |
| Vinegars (except apple cider vinegar) |
Tips for Sweeteners and Condiments:
- Even low FODMAP sweeteners should be used in moderation
- Many commercial sauces and condiments contain garlic and onion—read labels carefully
- Make your own salad dressings and sauces using low FODMAP ingredients
- Infused oils can add significant flavor without FODMAPs
Snacks and Convenience Foods
| High FODMAP Snacks (To Avoid) | Low FODMAP Alternatives |
|---|---|
| Pretzels | Popcorn |
| Wheat crackers | Rice crackers |
| Cashews | Peanuts |
| Potato chips with onion/garlic | Plain tortilla chips |
| Plain potato chips | |
| Dark chocolate (small amounts) | |
| Certified low FODMAP snack products | |
| Rice cakes with peanut butter |
Tips for Snack Consumption:
- Plain, unflavored versions of snacks are more likely to be low FODMAP
- Look for certified low FODMAP products for convenience
- Combine a low FODMAP carbohydrate with a protein source for a more satisfying snack
- Prepare portable snacks in advance to avoid being caught without safe options
Practical Implementation: Meal Planning and Recipes
Sample Low FODMAP Meal Plan
Here’s a sample one-day meal plan incorporating low FODMAP alternatives:
Breakfast:
- Porridge made with rolled oats and lactose-free milk
- Topped with firm banana slices and a sprinkle of cinnamon
- Lactose-free yogurt on the side
Mid-Morning Snack:
- Orange or kiwi fruit
- Small handful of walnuts
Lunch:
- Grilled chicken with quinoa salad (including zucchini, carrots, cucumber, bell peppers)
- Dressing made with olive oil, lemon juice, and herbs
- Rice crackers on the side
Afternoon Snack:
- Rice cakes with peanut butter
- Small bowl of strawberries
Dinner:
- Grilled salmon with mashed potatoes
- Steamed green beans and carrots
- Salad with lettuce, tomato, and cucumber with olive oil and lemon dressing
Evening Snack (Optional):
- Lactose-free milk or almond milk smoothie with strawberries and a small amount of maple syrup
Kitchen Staples for Low FODMAP Cooking
Building a well-stocked pantry with low FODMAP staples makes meal preparation easier. Here are essential items to keep on hand:
Pantry Staples:
- Garlic-infused olive oil
- Onion-infused olive oil
- Gluten-free pasta
- Rice (various types)
- Quinoa
- Gluten-free bread
- Oats
- Rice cakes
- Certified low FODMAP stock cubes or powder
- Canned tuna/salmon
- Canned lentils (rinse well before use)
- Tomato paste (no garlic or onion)
- Soy sauce (check ingredients)
- Vinegars (except apple cider vinegar)
- Pure maple syrup
- Table sugar
Refrigerator Staples:
- Lactose-free milk
- Lactose-free yogurt
- Hard cheeses
- Eggs
- Firm tofu
- Fresh herbs
- Lemon/lime
- Low FODMAP vegetables
- Low FODMAP fruits
Freezer Staples:
- Plain meat portions (chicken, beef, pork)
- Fish fillets
- Frozen berries
- Gluten-free bread (freezes well)
Simple Recipe Adaptations
Many traditional recipes can be adapted to be low FODMAP with simple substitutions:
Pasta Sauce:
- Traditional: Onion, garlic, canned tomatoes
- Low FODMAP: Garlic-infused oil, green parts of spring onions, canned tomatoes (check for no added garlic/onion)
Stir-Fry:
- Traditional: Onion, garlic, various vegetables, soy sauce
- Low FODMAP: Garlic-infused oil, green parts of spring onions, low FODMAP vegetables (bell peppers, carrots, bean sprouts), tamari or suitable soy sauce
Breakfast Cereal:
- Traditional: Wheat-based cereal with milk
- Low FODMAP: Oats or certified low FODMAP cereal with lactose-free milk
Sandwich:
- Traditional: Wheat bread, various fillings
- Low FODMAP: Gluten-free bread, suitable fillings (egg, hard cheese, plain meat, lettuce, tomato)
Curry:
- Traditional: Onion, garlic, various spices
- Low FODMAP: Garlic and onion-infused oils, green parts of spring onions, suitable spices (turmeric, cumin, coriander, etc.), certified low FODMAP curry pastes
Challenges and Solutions in Following a Low FODMAP Diet
Nutritional Concerns
One of the primary concerns with the low FODMAP diet is ensuring nutritional adequacy, particularly during the restriction phase. Here are potential nutritional challenges and solutions:
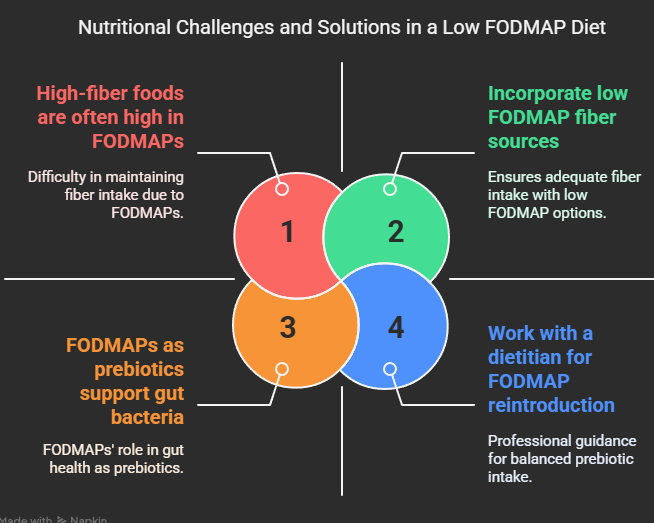
Fiber Intake:
- Challenge: Many high-fiber foods are also high in FODMAPs
- Solution: Focus on low FODMAP fiber sources like oats, quinoa, rice bran, firm bananas, oranges, strawberries, kiwi, and suitable vegetables
Calcium:
- Challenge: Restricting dairy can reduce calcium intake
- Solution: Use lactose-free dairy products, which retain calcium content, or calcium-fortified plant-based alternatives
Prebiotics:
- Challenge: FODMAPs act as prebiotics, feeding beneficial gut bacteria
- Solution: Work with a dietitian to reintroduce tolerated FODMAPs as soon as possible; consider low FODMAP prebiotic sources like firm bananas
B Vitamins:
- Challenge: Restricting whole grains may reduce B vitamin intake
- Solution: Include low FODMAP whole grains like oats and quinoa; consider fortified gluten-free products
Variety:
- Challenge: Restricted food choices can lead to monotonous eating
- Solution: Experiment with herbs, spices, and different cooking methods to create variety with permitted foods
Eating Out and Social Situations
Dining out while following a low FODMAP diet can be challenging but not impossible:
Restaurant Strategies:
- Research menus online before visiting
- Call ahead to discuss dietary needs
- Choose simple dishes that are easier to modify (grilled meats, fish, salads)
- Ask for sauces and dressings on the side
- Request modifications like “no onion or garlic”
- Bring your own salad dressing or sauce if necessary
- Focus on naturally low FODMAP cuisines (certain Japanese dishes, simple grilled options)
Social Gatherings:
- Eat a small low FODMAP snack before attending
- Offer to bring a dish you know you can eat
- Communicate your needs to the host in advance
- Focus on the social aspect rather than the food
- Have a brief, simple explanation ready if asked about your diet
Traveling on a Low FODMAP Diet:
Maintaining a low FODMAP diet while traveling requires thoughtful planning, but it’s absolutely achievable. Here’s everything you need to know to stay on track and enjoy your journey.
Preparation Tips
- Research Food Availability: Look into low FODMAP-friendly options at your destination.
- Pack Non-Perishable Snacks: Carry items like rice cakes, nuts (in appropriate portions), and certified low FODMAP protein bars.
- Choose Accommodation with Kitchen Facilities: This allows you to prepare meals as needed.
- Download the Monash University FODMAP App: Use it as an on-the-go reference.
- Carry a Translated Dietary Card: Essential for international travel to explain your dietary needs.
- Research Restaurants in Advance: Identify places that offer low FODMAP options.
- Bring Shelf-Stable Foods: Consider oatmeal packets, tuna pouches, or peanut butter.
Practical Travel Foods
- Rice cakes with peanut butter packets
- Firm, unripe bananas
- Hard cheeses (travel well for short periods)
- Individually wrapped gluten-free crackers
- Small portions of suitable nuts
- Certified low FODMAP protein bars
- Plain rice or corn-based cereals with lactose-free UHT milk
Psychological Aspects of Dietary Restriction
The restrictive nature of the low FODMAP diet, especially during the elimination phase, can impact mental health.
Common Challenges
- Food-related anxiety
- Social isolation
- Reduced enjoyment of eating
- Disordered eating patterns
- Stress around food choices
Supportive Strategies
- Work with both a dietitian and psychologist if needed.
- Focus on foods you can eat rather than restrictions.
- Join support groups (online or in-person).
- Celebrate small victories and symptom improvements.
- Practice mindful eating to enhance enjoyment of permitted foods.
As Dr. Jane Muir from Monash University says:
“The low FODMAP diet is not meant to be a forever diet. It’s a diagnostic tool to help identify your specific triggers, allowing you to liberalize your diet as much as possible while managing symptoms.”
Beyond FODMAPs: Complementary Approaches to IBS Management
While the low FODMAP diet is effective, combining it with other strategies can optimize results.
Stress Management Techniques
- Mindfulness meditation (reduces IBS symptoms by 38%).
- Gut-directed hypnotherapy (as effective as the low FODMAP diet for some).
- Cognitive Behavioral Therapy (CBT) for unhelpful thought patterns.
- Regular exercise and adequate sleep.
- Breathing exercises to activate the parasympathetic nervous system.
Medication Options
- Antispasmodics for abdominal pain and cramping.
- Laxatives or anti-diarrheal medications for bowel issues.
- Low-dose antidepressants for pain perception and gut motility.
- Gut-specific antibiotics for SIBO cases.
- Probiotics and digestive enzymes as needed.
Gut Microbiome Considerations
- Incorporate probiotic foods like fermented options (if tolerated).
- Gradually reintroduce prebiotic foods for beneficial bacteria growth.
- Include polyphenol-rich foods like berries and green tea.
Tailored Approaches for IBS Subtypes
- IBS-D (Diarrhea Predominant): Focus on soluble fiber from oats, limit fat intake, avoid caffeine/alcohol, and space out meals.
- IBS-C (Constipation Predominant): Stay hydrated, engage in gentle physical activity, introduce magnesium-rich foods like pumpkin seeds, and maintain regular meal timing.
- IBS-M (Mixed Type): Keep detailed records of triggers, balance fiber types, and personalize FODMAP thresholds.
Advanced Strategies for Long-Term Management
FODMAP Stacking
Be mindful of cumulative effects when consuming multiple low FODMAP foods from the same subgroup within 3–4 hours.
Reintroduction Strategies
- Test one FODMAP subgroup at a time using structured challenges.
- Document responses in detail to identify tolerances.
Periodic Reassessment
IBS triggers may evolve over time—reassess every 6–12 months with professional guidance.
Special Considerations
- Children & Adolescents: Work with pediatric dietitians to ensure proper nutrition while managing IBS symptoms.
- Vegetarians/Vegans: Focus on tofu, tempeh, fortified plant milks, and supplements if necessary.
- Pregnancy & Breastfeeding: Liberalize the diet under professional supervision to meet nutritional needs.
- Elderly Individuals: Simplify approaches while addressing age-related digestive changes.
Frequently Asked Questions
How long should I stay on the elimination phase?
Typically 4–6 weeks; consult a professional if no improvement is seen.
Can I follow this diet with other restrictions?
Yes, but it requires careful planning with a dietitian.
Will I need to avoid high FODMAP foods forever?
No, the goal is to identify triggers and reintroduce tolerable foods.
Can this diet cure IBS?
It’s not a cure but an effective management strategy.
What if I accidentally consume high FODMAP food?
Resume the plan at your next meal; one mistake won’t derail progress.
Conclusion
Managing IBS through dietary modifications like the low FODMAP diet is about knowledge, empowerment, and finding personalized solutions that work for you.
As Dr. William Chey states:
“The low FODMAP diet has revolutionized our approach to IBS management, giving patients unprecedented control over their symptoms.”
Take charge of your digestive health today—your journey toward better well-being starts here!
This format ensures clarity while retaining all details from your query file content!
Discover more from NutriIgnite UK
Subscribe to get the latest posts sent to your email.

Comments are closed.